
Hepatic progenitor cells are often distinguished as primary or small hepatocytes. These cells will not necessary become mature hepatocytes, but may in fact differentiate into other functional cells of the liver, such as bile duct cells ( 12, 13).
Hepatic progenitor cells found within the liver have already begun to differentiate, but still have several options before becoming destined to a specific cell line. Deciding which cell type to use is dictated by the need and desire for the cells to perform in a predicted manner, exhibiting certain characteristics. The various cell types that have been studied include stem cells, hematopoietic cells, oval progenitor cell and mature hepatocytes ( 9– 11). In the field of hepatic tissue engineering, choosing cell type and cell source is important because it is necessary to choose cells that demonstrate the particular phenotype of interest. This review has presented some directions that the field of liver tissue engineering is heading. Advances in polymer chemistry have facilitated the engineering of synthetic matrices that can be precisely manipulated with regard to physical and mechanical characteristics. However, the challenge remains to develop robust protocols, to generate functional hepatocytes from stem cells suitable for the transplantation.Ī complementary key ingredient in regenerative medicine and tissue engineering is to make a use of biologically compatible scaffolds that can be readily adopted by the body system without harm ( 6). Today, there are different studies showing hepatogenic differentiation capacity of the stem cells ( 3– 5). Self-renewal is a unique property of stem cells that gives multi-potential differentiation ability to them. Considering the proliferation activity and differentiation potential of cells, stem cells are practically promising. For successful tissue regeneration, the cells constituting tissues to be regenerated are necessary. Tissue engineering proves to be a temporary treatment for patients suffering from hepatic failure ( 2). However, the efficacy of liver transplantation is limited by the shortage of available organ donors, risk of rejection, infections, and other complications caused by the lifelong immunosuppression ( 1). At present, liver transplantation is the only therapeutic option for patients with end-stage chronic liver disease and severe liver failure. However, there are not enough organ donors.Īt the moment, there are about 700 patients waiting to have a liver transplant in Iran, but the number of liver donors is less than 200. Currently, there are many people waiting to have a liver transplant.
Hepatocyte tissue engineering scaffold electrospinning full#
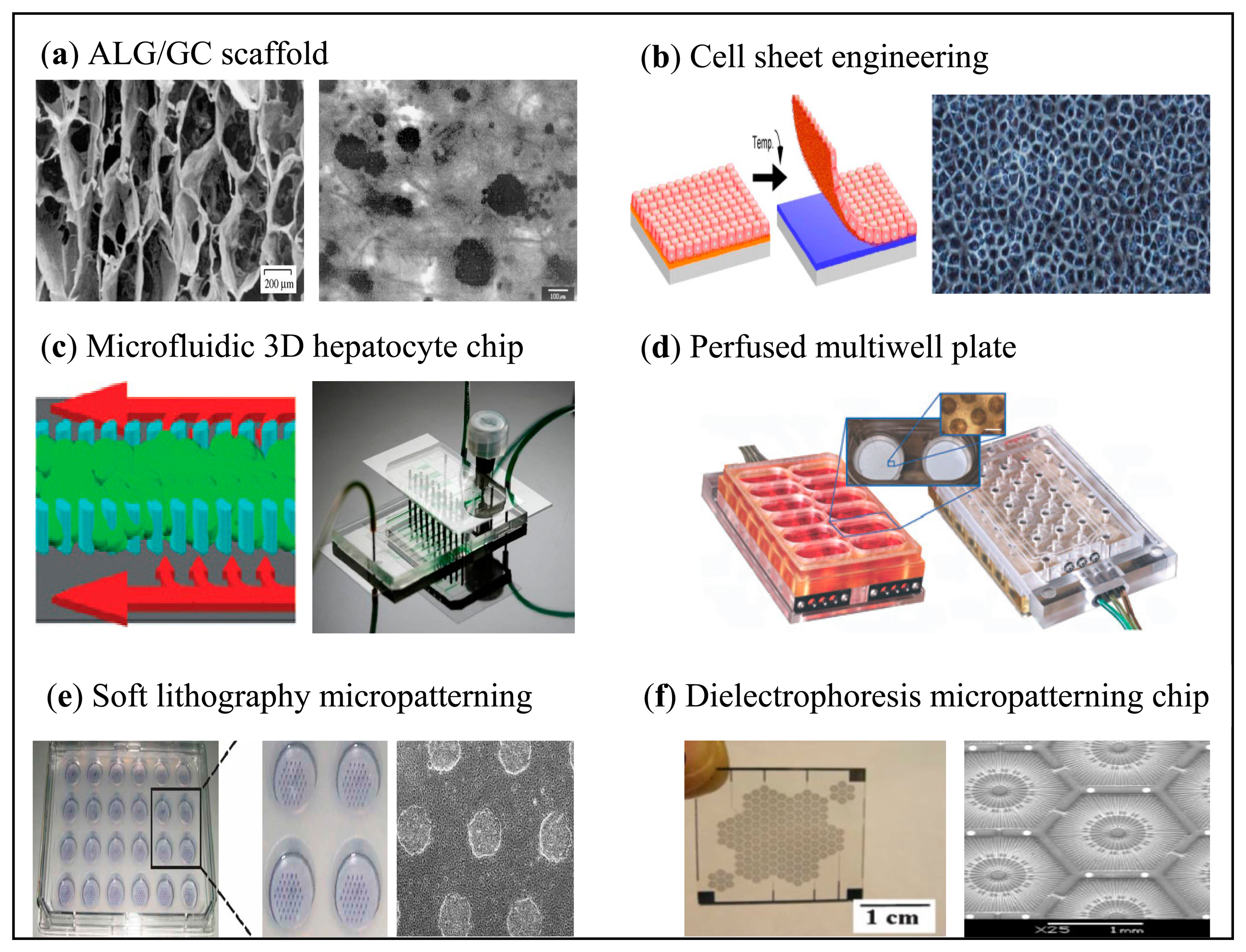
Many of those in need of a transplant have suffered from full hepatic failure caused by disease, genetic complications or adverse drug reactions. In this review, we have presented different concepts in using cell /scaffold constructs to guide hepatic tissue engineering.Įvery year, the number of patients needing a hepatic transplant increases. In recent years, different scaffolds have been used for liver tissue engineering. However, using suitable scaffolds is an important key to achieving the necessary functions required for hepatic replacement. Today, hepatogenic differentiation of stem cells has created trust and promise for use of these cells in hepatic tissue engineering and liver replacement. Yet many challenges must be overcome such as scaffold choice, cell source and immunological barriers. Regenerative medicine and tissue engineering require two complementary key ingredients as follows: 1) biologically compatible scaffolds that can be readily adopted by the body system without harm, and 2) suitable cells including various stem cells or primary cells that effectively replace the damaged tissues without adverse consequences. Hepatic Tissue Engineering is a step toward alleviating the need for organ donors. Due to decrease in the number of organ donors, many in need of transplantation continue to remain on the waiting list. Currently, liver transplantation is the most common therapeutic option for patients with end-stage chronic liver disease. Severe hepatic failure accounts for many deaths and raises medical costs each year worldwide.


 0 kommentar(er)
0 kommentar(er)
